At least one in six couples now need medical help to have a baby…and for half of them the problem is the result of poor sperm quality. Infertility specialists fear this growing problem among men is bringing us closer to the day when most couples will need medical help to have a family.
This week, a major French study revealed sperm counts and quality have fallen sharply since the Nineties.
It is believed the trend is linked to diet, lifestyle and ‘gender-bending’ chemicals. The researchers, who used data from 126 fertility treatment centres, said their conclusions constitute a ‘serious public health warning’. But what is being done to alleviate the problem?
So far, it seems, very little.
Australian doctors are barely addresses the problem of male infertility, choosing instead to focus on the woman if a couple seek treatment over their inability to conceive.
The question must be raised, ‘Why do male doctors continue to lay blame for infertility on women?’
Do women themselves automatically assume infertility is their fault? Or could the driving factor be that invasive and complex fertility treatments for women are hugely lucrative for those carrying them out?
Most hospitals operate from a standpoint that men are unquestionably fecund and virile and it is somehow inappropriate to humiliate them with intrusive tests.
Some women will visit their GP after struggling for 18 months to conceive, the doctor referred them to a gynaecologist — by definition a specialist in women’s problems, even if the woman already had a son.
Causes of male infertility include antibiotics, drugs, alcohol, obesity, fevers, stress and abstinence from sex for more than a few days
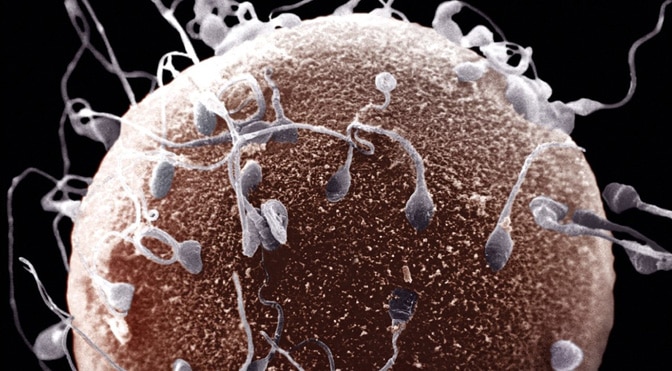
Of an average 200 million to 500 million sperm released during male orgasm, only 50 to 100 will complete the journey to the egg without getting lost or dying from exhaustion. The journey can take up to six days.
Only a few dozen will have sufficient strength left to attempt to drill into the egg and only one will make it.
This natural selection — ensuring only the healthiest sperm succeed — has propagated the human species for thousands of generations.
It is now failing before our eyes, but the problem remains a taboo which many men — including doctors — find too embarrassing to discuss.
It seems they would rather subject women to pointless and intrusive tests than risk damaging fragile male egos.
This can mean even a man with a lot of sperm can still be infertile because it is too damaged to penetrate a female egg. The so-called ‘sperm comet’ test uses a specialised light field which shows intact DNA in a sperm cell.
It gives a more accurate prediction of fertility than a straightforward sperm count, and can be performed with no involvement from the man other than providing a sample.
Fertility tests routinely performed on women, on the other hand, are far more painful, invasive and expensive. Apart from taking blood samples to check hormone levels, dye is injected into the ovaries to check eggs are being produced.
The womb, the tubes from the ovaries and the ovaries themselves are probed under general anaesthetic using keyhole surgery, and a different operation may be ordered to scrape tissue from the lining of the womb for analysis.
Evidence showing that sperm concentrations had halved since the Forties first began to emerge 20 years ago.
Many scientists questioned the testing methods used in these early studies, but since then an avalanche of other research has shown sperm quality deteriorating year on year.
Incidence of cancer of the genital organs in young men has also inexplicably doubled since the Seventies.
Research published only last month shows more than one in 20 baby boys is now born with undescended testes, trebling the risk of testicular cancer which usually strikes in young adulthood and often results in infertility.
We now know chronic unfitness and obesity can also sabotage the reproductive capacity of men, and long-term harm from cigarettes can be passed from smoking father to non-smoking son.
It’s also known that by-products from some plastics that mimic the effects of female hormones are damaging to sperm, as are by-products from car pollution.
‘There are lots of reasons to be worried about this,’ says Marco Gaudoin, medical director of the Glasgow Centre for Reproductive Medicine.
‘We now have something like 80,000 new chemicals introduced in the Western world in the past century. We have rivers where all the fish are female.
‘Even if you have a man with a normal sperm count by conventional measures, you might still find there are high levels of damage to the sperm DNA, and we don’t know what’s causing it.’
Although other doctors acknowledge the growing fears over environmental factors, many still maintain the biggest cause of the infertility epidemic is the cult of self-fulfilment.
On one hand we are now increasingly promiscuous, suffering epidemics of chlamydia and other sexually-transmitted diseases that affect fertility.
On the other hand, couples are leaving attempts to become parents later and later, allowing age and increased exposure to lifestyle risk factors to take their toll.
by Susan Floyd